Pomona vs. the Pandemic Part 5
Part 1: Pomona vs. the Pandemic
Part 2: Going Virtual
Part 3: Bittersweet 16
Part 4: Job-Hunting in the Pandemic
EMERGENCY ROOM PHYSICIAN Jonathan Gelber ’10 is on the front lines battling the coronavirus (COVID-19) pandemic at Highland Hospital in Oakland, California. Jennifer Doudna ’85, internationally famous for the CRISPR-Cas9 gene-editing technique, is establishing a high-capacity coronavirus testing lab on the University of California at Berkeley campus. And Victoria Paterno ’75 P ’07, an assistant clinical professor in pediatrics at UCLA Medical Center who had retired from private practice, volunteered to return for COVID-19 duty. Those are just a few of the many Sagehens across the country who are responding to the pandemic. Here are a few of their stories in their own voices.
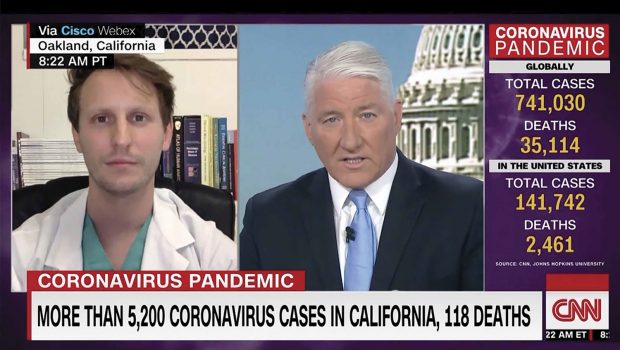
Jonathan Gelber ’10
Emergency Room Physician, Oakland, CA
“We do care predominately for vulnerable patients, people of unstable housing or frankly, homeless,” Gelber told CNN on March 30. “When we work to plan discharges, when we tell people things like ‘shelter in place,’ [we’ve learned] to make sure people have a shelter to ‘shelter in place’ in. We think it’s a lot easier to tell somebody like me to go hang out at home for two weeks and get food delivered. It’s a little harder when the patient is a 55-year-old gentleman who lives in a tent encampment under the 45th Street bypass, and with 15 other people. So we’ve learned how to plan for that and see our problems ahead of time before they arise. That’s saying, hey, how do we keep the curve flat, how do we keep patients like this from infecting other patients at shelters, at homeless encampments, as well as the general patient population? And how do we keep the people in the emergency room safe from infecting each other in the lobby?”

Zack Haberman ’10
Zack Haberman ’10
Emergency Room Physician, Stockton, CA
“My ER serves a diverse community, including a large elderly and socioeconomically underserved population. I am seeing the number of COVID patients continue to grow. While I can draw on what I’ve learned from basic science at Pomona, medical school and residency, the scariest part of the virus is how much is unknown. In many ways, I am used to that—my job is to see patients with an unknown illness or problem and make life-or-death decisions based on incomplete information. However, the more I see and read about the virus, it doesn’t seem to respond in the same way that other serious heart and lung emergencies do. Because of that, we still don’t know the best way to treat patients—especially the sickest ones. And unlike most emergencies, it is putting myself, my co-workers and our families at risk. I’ve already had to take care of my colleagues who have fallen ill from COVID, and I get a pit in my stomach knowing that there will be more to come.”

Vian Zada ’16
Vian Zada ’16
Fourth-year Medical Student, Georgetown University
“Medical students across the country are helping out with the response in virtual ways. For me, I am part of the MedStar Telehealth Response Team and, with other students, am calling thousands of patients with their test results. I am also a coach with our school’s disaster preparedness exercise, and leading Zoom sessions for first-year medical students. I also have an Instagram page @studentsagainstcovid, which I am managing with some health professionals in the San Diego area, where I grew up. We are hoping to target younger audiences with information on social distancing and disease prevention.”

David Siew ’98
David Siew ’98
Internal Medicine Physician, Kirkland, WA
“Our hospital identified the first large-scale outbreak of COVID-19 disease in the United States after noting an influx of patients with unexplained respiratory disease from a local care facility. Up until that point, COVID-19 still felt a world away and none of these patients had the primary risk factor: international travel. We were shocked to discover ourselves at the initial national epicenter of the pandemic. I am amazed and humbled by the mobilization of our hospital and the multidisciplinary effort of every member of our organization to care for the community. My group continues to treat many hospitalized patients with the disease and has compiled the lessons we are learning for other health care providers. … The growing and evolving body of knowledge regarding COVID-19 requires providers to assimilate new information on a daily basis. Since there are many uncertainties, we have to collaborate with others and form our own critical conclusions on which to base our testing and treatment strategies.”

Daniel Low ’11
Daniel Low ’11
Famiy Medicine Physician, Seattle, WA
“I think it is critically important to highlight the disproportionate effect that COVID-19 has on marginalized communities. Certainly, COVID-19 has touched virtually everyone, but the manifestations are exacerbating existing socioeconomic and racial inequities in our country. Community health centers are being hit particularly hard and are having particular difficulty in serving the most disenfranchised individuals in our communities. Without a critical lens focusing on the most vulnerable, things as seemingly utilitarian as the ethical rationing of limited ventilators will ultimately worsen healthcare disparities because criteria for respirators often focus on the absence of chronic conditions, and yet we know that structural violence and systemic racism have resulted in communities of color and economically disadvantaged people having higher rates of chronic conditions at baseline. I’m trying to push an agenda that focuses on and responds to the most underserved during this crisis, as we already have emerging data demonstrating that these communities are the most hard-hit.”

Kate Dzurilla ’11
Kate Dzurilla ’11
Nurse Practitioner, Brooklyn, NY
“I live on the Upper West Side, and look forward to 7 p.m. every night when we open our windows to hear cheers, applause, trumpets, bells, dogs barking, etc. Each night over the past week the cheers are growing louder. I cheer for my colleagues working in medicine, but also for the other essential personnel that are making this time in our lives easier, like those working in grocery stores, hardware stores, and bodegas, and delivering food and driving public transportation that helps me get to work. It reminds me that we’re all in it together, and that despite how unbelievable and painful this time is, we still feel hope and optimism.”

Vicki Chia ’08
Vicki Chia ’08
Chief Resident in Obstetrics and Gynecology, Boston, MA
“I have borne witness to the impact that the COVID-19 pandemic has had on the birth experiences of patients whose communities have historically experienced denials of reproductive freedom. Restricting the presence of a patient’s labor support person(s), disclosing their diagnosis of COVID-19, and making the recommendation of separation from their baby feels like an emotional assault on a new parent, especially one who has limited resources in terms of housing and childcare. Additionally, my fellow health care providers and I are experiencing the shortage of personal protective equipment (PPE) through hospital policies that ration or require reuse of PPE, and limitations in testing capacity have resulted in late diagnosis and delayed identification of health care worker exposures.”

Shennan Weiss ’00
Shennan Weiss ’00
Neurologist, East Brooklyn, NY
“As a neurologist I was consulted for cases of stroke, seizure and confusion. We saw an increase in the number of our consultations as the COVID-19 pandemic grew. We saw at least five cases of catastrophic large blood vessel strokes in patients under 60 who were infected with COVID-19. On at least one occasion, we intervened with a thrombectomy revealing a larger than normal blood clot. Not all of these patients survived as a result of related respiratory complications. Those who did survive were discharged to nursing facilities often still suffering from debilitating hemiparesis and aphasia.”

Johanna Glaser ’10
Johanna Glaser ’10
Fourth-year Medical Student, UC San Francisco School of Medicine
“I just finished a rotation in a skilled nursing facility at the local VA [Veterans Affairs] hospital. All of my patients during this time, men over 70 years old with comorbidities, were among the highest risk for serious illness and death if exposed to SARS-CoV-2. It’s been devastating to see the fatality rate of this pandemic among the elderly, especially those residing communally, with about a fifth of all deaths in the U.S. due to COVID-19 being linked to nursing facilities. Luckily, not a single occupant of the facility where I was on rotation had any worrisome symptoms nor had tested positive for the virus. This, however, came at the cost of extreme isolation for this otherwise highly sociable group of men. …
“I hope that we can take this moment to reexamine how we deliver health and essential services in our country, with a new focus on marginalized populations and health equity. … In the medical context and more broadly, let us take this unprecedented event as an opportunity to avoid unnecessary suffering and inequality in the future.”
